«I am truly confused» Georgia exclaimed while leaving the doctor's office. « The doctor told me that I suffer from Complex Regional Pain (or Reflex Sympathetic Dystrophy) and has given me a bunch of painkillers (analgesics) to cure me! When I followed his instructions I felt worse! I called my doctor disappointed and expressed that my pain was not getting better as a result of the medication. I felt that no one understood me and that they were trying to get rid of me. They told me that my pain was due to the fact I was working too hard. I decided to take their advice and stay home from work but I felt even worse».
Georgia D, 35 yr old, Advertisement Executive, Chronic pain patient
Does the above experience ring a bell? Pain is peculiar, in that medication doesn't always work, as is the case in other circumstances! Many of us have tried painkillers, physiotherapy, biofeedback, surgery and a million more techniques doctors promised us would work, cure our pain, but our pain is still there! When we exercise a lot / or at least as much as we want to, it hurts, however our life is often put on standby waiting for the pain to disappear. If we put a halt on our daily tasks we end up feeling overwhelmed by thoughts related to our pain. The emotions are intense but at the same time a glimmer of hope that «maybe sometime in the future my pain will reside» still sometimes appears. In addition, health professionals and family alike often give the message that we «must go on and fight this pain; finally we will win the fight». The most difficult part of chronic pain however, is accepting that pain might never go away! In many instances, the thought that « I will have to live with pain for the rest of my life » creates an internal battle, and even more distress. It's truly terrifying thinking that pain will never go away!
What is chronic pain, however? In the past, the answer people got was: « it's all in your head! ». Today, despite the lack of objective tools to measure pain, chronic pain has been defined as:
• When there exists current damage/irritation (or old damage) to the body's tissue,
• When pain intervenes in the life of the person and impairs their daily functioning over and above the expected period taken for a wound to heal (e.g. for many weeks or at least 3 continuous months),
• The pain is potentially associated to a progressive disease (e.g. arthritis, cancer etc.).
International Association for the Study of Pain [IASP], 1994.
• When there exists current damage/irritation (or old damage) to the body's tissue,
• When pain intervenes in the life of the person and impairs their daily functioning over and above the expected period taken for a wound to heal (e.g. for many weeks or at least 3 continuous months),
• The pain is potentially associated to a progressive disease (e.g. arthritis, cancer etc.).
International Association for the Study of Pain [IASP], 1994.
What do the above points really mean?
 |
For us to understand pain we must ask ourselves what pain is not. Acute pain, as opposed to chronic pain triggers our body's alarm system, telling us that «something sinister is going on». People usually feel acute pain following some sort of trauma or tissue damage. In this instance, our alarm system is useful, in that it prevents further damage from occurring to our body. Acute pain can also be called pathological pain because having experienced an accident sends signals to our nervous system which ends up travelling to our brain, which in turn decodes the signals, telling us that we feel pain. In chronic pain, pain signals never stop even after the wound has healed, we feel jolts as if a car just passed by, trembling as if someone was walking on a wooden floor, we feel «dagger» pains or «nails» piercing. Chronic pain occurs when our body is not working properly, it is in a constant state of alarm, and it's as if «a siren is whaling continuously as if in a real emergency». Chronic pain is also called «neuropathic pain» and it's caused by our brain interpreting pain derived from original tissue damage and thinking that «something must be done» or «our life is in danger». The difference between acute and chronic pain is that the latter usually poses «no immediate threat to the body». Chronic pain typically starts from an episode of acute pain but its intensity does not necessarily go away following the passage of time or post treatment. |
The International Association for the Study of Pain says that chronic pain is an « unpleasant physical and emotional experience, a combination of real and virtual tissue damage, that can last for longer than the expected time needed for the damage to heal » (Merskey & Bogduk, 1994, 210-211). When describing chronic pain, we refer to:
Something that lasts a long time (e.g. months or/and years), Followed by potential illness, Or that is associated with tissue damage that has not healed despite the passage of time (IASP, 1994).
 |
Pain can be classified into three groups depending on its origin, α) nociceptive, following tissue damage, b) neuropathic, where there is damage to the peripheral or central nervous system or c) psychogenic, where serious mental illness such as psychosis or severe depression are present. Most symptoms related to chronic pain, can be attributed to pathological disorders, nervous system disorders or psychological disorders. Many studies have shown that patients who experience similar back injuries such as tissue inflammation, muscular fibrosis and disc herniation either experience or do not experience chronic pain. Contrary to what is believed there is little connection between tissue damage and the pain we feel. This is why regular checkups are necessary! |
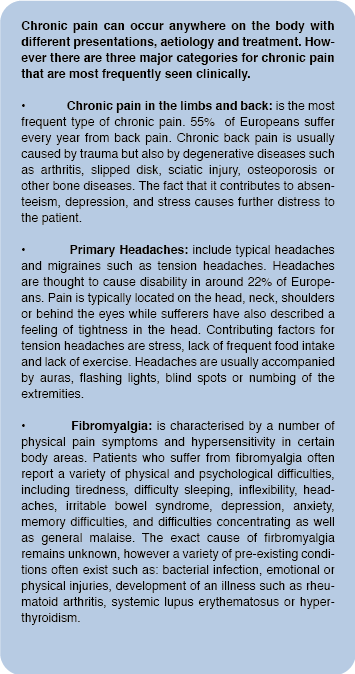
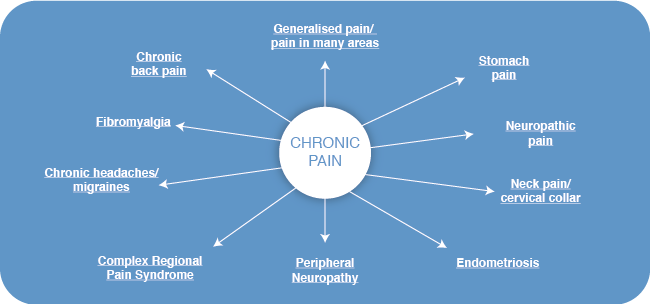
There are many examples of chronic pain which are musculoskeletal in nature such as whiplash (often a result of trauma to the neck following a car accident), or fibromyalgia (characterised by pain and tiredness) or migraines and tension headaches, where there is little proof of tissue damage. Over 85% of people with back pain have no pathological explanation. Despite this pain is often severe, it causes anxiety and inhibits functionality in the person experiencing it. Taking the example of chronic headaches, rarely can one find tissue damage, despite appropriate medical tests, that can be attributed to the sufferer's pain experience. People who experience pain oftentimes get the message from their doctor, significant others or family members that they are indeed exaggerating their experience. We are in disagreement with this statement and believe that pain is in fact a reality for pain sufferers. Millions of people suffer chronic pain and new non pharmacological treatments can help people limit the impact pain has on their life. Psychological therapies are a vital part of rehabilitation for people experiencing chronic pain. The treatment effectiveness for psychological therapies is substantial in pain patients given positive influence on quality of life. The ALGEA team believes in the induction of psychological therapies into mainstream medical and rehabilitation facilities for pain sufferers. ALGEA aims at making this dream a reality for chronic pain sufferers.
 |
Pain is thought to be a «subjective experience». Pain is experienced differently by different people, even following relative objective tests of pain intensity. Pain can influence one's social and family life and often results in avoidance behaviour that limits one's life.
Independent of the nature or causes of pain people don't seek medical advice for their pain as such, but for the impact their pain has on their life either though feelings of stress, depression or the impact on their quality of life. The meaning attributed to pain often, influences the way people react to it.
It seems that people with chronic pain who accept their situation, who actively do things in spite of their pain, who perceive doctors as useful and who believe that they are not seriously impaired as a result of their pain function better in all areas of their life. |
Pain influences both the person and those around them. Other people's reactions as well as the culture and society in which we live, play a vital role in one's pain experience. For example, older people experience pain differently than younger people, given beliefs about the normal consequences of ageing. On the other hand, teenagers who experience chronic pain are prone to exhibit more psychological disorders and physical disability due to the impact pain has on daily activities (e.g. school, friends etc.), generalised anxiety and worry is also increased in the teenage population. Childhood chronic pain, like adult pain, is not purely and directly related to tissue damage or progressive disease. Childhood chronic pain is thought of as «less real» compared to adult pain given the fact that it is highly influenced by psychosocial factors. As a child grows older, it learns how to cope with pain by mimicking behaviour from its immediate family, culture and interrelationships with important others.
The relationship between a pain sufferer and their family members plays a vital role in pain expression. Studies suggest that positive attention and support shown towards the person experiencing pain (e.g. helping them sit down, doing all the housework) leads to more pain in the sufferer as a result of increased preoccupation with pain signals and an increased sense of helplessness. At the same time, when family members express themselves negatively (e.g. showing disbelief, mocking or ridiculing etc) this leads to an increase in both anxiety and depression symptoms.
The real challenge for patients, relatives and health care professionals, is finding a middle ground. The good news is that despite the presence of pain and the many hours spent trying to heal from pain, we can indeed find, a way to change our perception of pain. We don't need to ignore pain, make it go away or even find a way to get the better of it; ultimately we know it's still there! Our aim is to create a balance between acceptance and change. The ALGEA project aims at creating a new way of being, supporting patients to «manage their pain» rather than trying to lessen their pain sensation. Psychological factors undoubtedly play a crucial role in chronic pain and it is time that both Greece and Cyprus incorporate psychological care in their rehabilitation programmes. The ALGEA team commits itself to aid in the transformation of valid therapeutic techniques necessary for the treatment of patients with chronic pain.
Should you want to take part at any stage of our research Please contact us at This email address is being protected from spambots. You need JavaScript enabled to view it. or telephone on 00.357.22892024.